Protože zapáchající střevní metabolity překračují bariéru střevní stěny a jater, vylučují se potem a dechem. Výsledné příznaky se nazývají bromhidróza a halitóza.

Jazyky: BG | ZH | ZH-CN | ZH-HK | ZH-TW | CS | CS-CZ | DA-DK | NL | NL-BE | NL-NL | EN | EN-AU | EN-BE | EN-CA | EN-CN | EN-EN | EN-DE | EN-IE | EN-MY | EN-NZ | EN-NG | EN-PH | EN-ZA | EN-GB | EN-US | ET-EE | FI | FI-FI | FR | FR-BE | FR-CA | FR-FR | FR-CH | DE | DE-AT | DE-DE | DE-CH | EL | EL-GR | HU | HU-HU | IT | IT-IT | IT-CH | JA | JA-JP | KO-KR | NB | PL | PL-PL | PT | PT-BR | PT-PT | RO-RO | RU | RU-RU | SK | SK-SK | SL-SI | ES | ES-AR | ES-CO | ES-LA | ES-MX | ES-PE | ES-ES | ES-US | ES-VE | ES-XL | SV | SV-SE | TR | TR-TR | UK-UA |
Jak se přihlásit?
Pacienti s IMBS se mohou zapsat do mezinárodního registru pacientů, který je umístěn na adrese CoRDS (Sanford Research) platforma.
Podrobnější informace o registru pacientů najdete v následujícím letáku: Informační leták o registru pacientů
Vřele doporučujeme každému pacientovi, aby se do registru přihlásil, protože soubor údajů z tohoto registru pacientů je základnou, o kterou se výzkumníci opírají při zásadních rozhodnutích o tom, jaká vyšetření a jaký druh vyšetření u pacientů se vzácným onemocněním provést.
Poznámka:
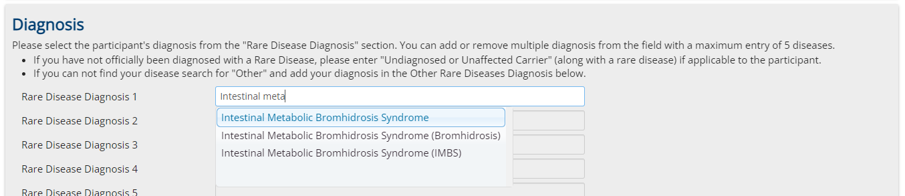
Je velmi důležité zvolit na první registrační stránce "Intestinal Metabolic Bromhidrosis Syndrome" jako vzácné onemocnění. (Zvolte ji také v případě, že se jedná pouze o podezření, které ještě nebylo diagnostikováno).
Zpráva:
Automaticky aktualizovanou zprávu založenou na podmnožině údajů z rejstříku si můžete stáhnout z následujícího odkazu:
Nenechávejte nás dělat práci samotné! Nebuďte pasivní - jednejte! Jednejte společně s námi!
Jsme lidé jako vy, kteří pracují na všech frontách, aby byla tato nemoc rozpoznána, zavedena v medicíně a vyřešena!
Spojte s námi síly, podpořte nás vším, čím nás můžete podpořit!
Řekněte všem, na které si vzpomenete, o tomto textu, o této skupině a o našich cílech! Řekněte jim, aby se přidali!
Nikdo za to nedostane peníze, ale možná se nám všem vrátí život, společenský život, pracovní život, všechno!
Sdílejte všude odkazy na naši komunitu, spojujte lidi - připojte se k naší alianci, buďte členem po našem boku!
Neváhejte, neběhejte sami, podpořte nás a nechte se námi podpořit!
Nebuďte pasivní - jednejte!

