Como los metabolitos intestinales olorosos atraviesan la barrera de la pared intestinal y el hígado, se excretan en el sudor y el aliento. Los síntomas resultantes se denominan bromhidrosis y halitosis.

Idiomas: BG | ZH | ZH-CN | ZH-HK | ZH-TW | CS | CS-CZ | DA-DK | NL | NL-BE | NL-NL | EN | EN-AU | EN-BE | EN-CA | EN-CN | EN-EN | EN-DE | EN-IE | EN-MY | EN-NZ | EN-NG | EN-PH | EN-ZA | EN-GB | EN-US | ET-EE | FI | FI-FI | FR | FR-BE | FR-CA | FR-FR | FR-CH | DE | DE-AT | DE-DE | DE-CH | EL | EL-GR | HU | HU-HU | IT | IT-IT | IT-CH | JA | JA-JP | KO-KR | NB | PL | PL-PL | PT | PT-BR | PT-PT | RO-RO | RU | RU-RU | SK | SK-SK | SL-SI | ES | ES-AR | ES-CO | ES-LA | ES-MX | ES-PE | ES-ES | ES-US | ES-VE | ES-XL | SV | SV-SE | TR | TR-TR | UK-UA |
¿Cómo inscribirse?
Los pacientes del IMBS pueden inscribirse en un registro internacional de pacientes que se encuentra en el CoRDS (Sanford Research) plataforma.
Encontrará información más detallada sobre el registro de pacientes en el siguiente folleto: Folleto informativo sobre el registro de pacientes
Recomendamos encarecidamente a todos y cada uno de los pacientes que se inscriban en el registro, ya que el conjunto de datos de este registro de pacientes es una base en la que se basan los investigadores para tomar decisiones fundamentales sobre una investigación y qué tipo de investigaciones en una cohorte de pacientes con enfermedades raras.
Nota:
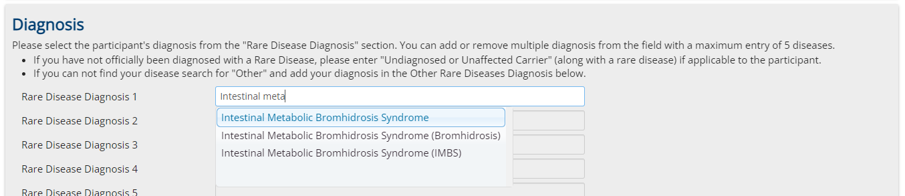
Es muy importante elegir en la primera página de registro "Síndrome de Bromhidrosis Metabólica Intestinal" como condición de enfermedad rara. (También elija esto en el caso de que sólo se sospeche y no se diagnostique todavía)
Informe:
Puede descargar un informe actualizado automáticamente basado en un subconjunto de los datos del registro en el siguiente enlace:
¡No dejes que hagamos el trabajo solos! No seas pasivo, ¡actúa! Actuad con nosotros.
Somos personas como tú, que trabajamos en todos los frentes para que se reconozca esta enfermedad, se establezca en la medicina y se solucione.
¡Únete a nosotros, apóyanos con todo lo que puedas apoyarnos!
Cuéntale a todo el mundo que se te ocurra sobre este texto, sobre este grupo y sobre nuestros objetivos. Diles que se unan.
Nadie recibe dinero por esto, pero quizá todos recuperemos nuestra vida, nuestra vida social, nuestra vida laboral, ¡todo!
Comparta enlaces en todas partes con nuestra comunidad, reúna a la gente: ¡únase a nuestra alianza, sea un miembro junto a nosotros!
No lo dudes, no corras solo, ¡apóyanos y déjate apoyar por nosotros!
No seas pasivo, ¡actúa!

